PCOS Awareness: My Diagnosis
Being diagnosed with PCOS in 2015 has definitely turned my world upside down. I view my health in a completely different way, my diet is significantly different, and I have a whole new set of challenges that I’m dealing with daily.
Since September is PCOS Awareness month I wanted to share my story on how I was diagnosed with it because I think it’s important to understand how easily this can be overlooked if you’re not trying for a baby. With my experience, I honestly don’t know if I would have been properly diagnosed if it weren’t for me having trouble conceiving.
I also think it’s crucial to be aware of how much you have to advocate for yourself because unfortunately, the medical community isn’t so understanding. I’ve done so much research, reading, listening to podcasts, etc. all on my own in order to learn how I needed to adjust my diet and lifestyle. I’m still constantly learning.
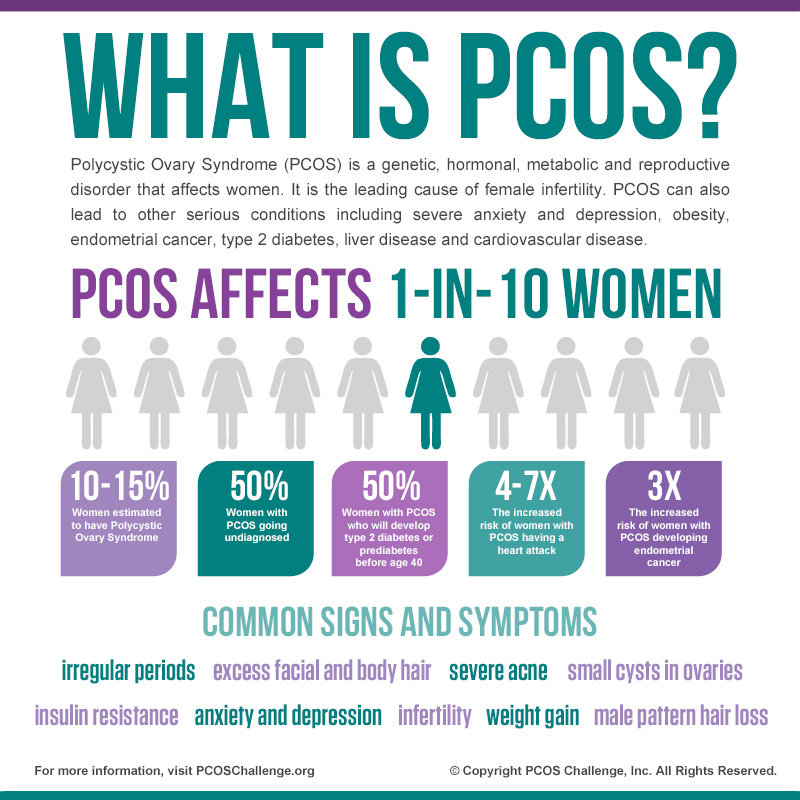
What is PCOS?
PCOS (Polycystic Ovary Syndrome) is a hormonal disorder that causes a variety of symptoms including acne, difficulty losing weight, excess hair growth, fertility issues, and more. While the very meaning of PCOS is multiple cysts, you don’t necessarily have to have multiple cysts in order to be diagnosed. In order to be diagnosed with PCOS you have to meet at least two out of the three criteria:
- Multiple cysts on your ovaries
- High androgen levels (DHEA, testosterone, androstenedione)
- Irregular menstrual cycles and/or difficulties ovulating
The jury’s still out on what exactly causes PCOS, but there are a couple possibilities: genetics, heredity, and a defect in a hormone-producing organ. There’s no cure for PCOS, but there are ways to manage it and reduce symptoms.
Background
In May of 2014 my prescription for the pill ran out, and I chose not to refill it. I had been on the pill for 9 years at that point, and we wanted to begin the process of starting a family (slowly). In the months that followed we go from using condoms to using no protection; we were NTNP (Not Trying, Not Preventing).
Upon celebrating our 4th wedding anniversary we decided to start officially TTC (Trying To Conceive). In my mind, this meant paying attention to when I was ovulating, tracking my BBT (Basal Body Temperature), and whatnot. The next couple of months I had difficulties getting a read on the ovulation tests, and that was also when I noticed I was having very irregular periods.
You can imagine how frustrating it is to be trying for a baby, being weeks late for your period, and no positive pregnancy test.
Meeting with My Doctor
The definition of infertility is the failure to get pregnant after having unprotected sex for at least a year. I was only 4 months in to really trying, but it was enough to have me concerned. Because of how my health insurance works, I couldn’t go directly to my OB. Instead, I had to go through my PCP, or as Joshua and I liked to call him Dr. Asshole (he had THE worst bedside manner).
I met with him to discuss my difficulties getting pregnant, so he sent me out for some labs. He also had Joshua get some testing done to rule out any Male Factor Infertility. Joshua checked out just fine, and as for me, all they told me was I had a Vitamin D deficiency. Simply take an extra Vitamin D3 supplement. No other instruction. 😐
This is where I realize looking back I should have started advocating for myself. I was able to see my lab results online, and my doctor didn’t bother to point out I was prediabetic. Fertility issues, prediabetes, irregular periods, acne, my weight going up over the years… these were all signs of PCOS. How was I suppose to know? I didn’t, and that’s why I was relying on my doctor to fill in the missing pieces. At the very least he should have put me on Metformin.
Since all I was told was just take an extra supplement and continue doing what I was doing, that’s how I proceeded. I figured I’d just wait it out a couple more months until I could see my gynecologist for my annual lady exam.
My Diagnosis
Three months later conditions did not improve. By the time I saw my gynecologist it had been 45 days in between cycles.
I had been using the app Glow to track all the things, and in their community, I kept seeing PCOS pop up in conversations, but I never really looked into it. I started to research it and suspected I might have it, but I wanted to see what my gyno said.
She sent me out for additional labs, one of which was to test my hormone levels. My follow-up visit revealed I had high testosterone levels. Between that and all the other symptoms, I was officially diagnosed with PCOS.
My gyno suggested I try losing 10% of my weight and see if that helps jumpstart things. Except as I later on found out, the trouble with PCOS is you have difficulty losing weight. Reducing weight can reduce symptoms, but it’s all the more challenging when you have something that makes it difficult to lose weight to begin with!
Moving Forward with PCOS
After consulting with two doctors, my instructions were to take an extra 4,000 IU of Vitamin D3 and lose 10% of my weight. Oh, and just keep trying. THAT WAS IT. No mention of supplements or medication (like Metformin), aside from the D3. No mention of consulting a nutritionist or Reproductive Endocrinologist (RE). No further recommendations.
After that, I was all on my own.
Unfortunately, my experience is pretty common.
Despite the fact that PCOS was first identified and researched in 1935 and the CDC has estimated it affects some 6 to 12 percent of adult women in the United States, many doctors still don’t recognize the symptoms. Women with PCOS and similar conditions like endometriosis and uterine fibroids, Ottey says, “have been told to suffer in silence.” Additionally, because PCOS often causes obesity or weight problems, many women with PCOS experience not just sexism but what Ottey calls “weight bias” in the health-care system. “Many women and young girls are told, ‘Oh, it’s all in your head. Just eat less and exercise more,’” says Ottey, who herself recalls being initially instructed by an endocrinologist to lose weight and come back in six months.
– How Women’s ‘Health-Care Gaslighting’ Went Mainstream
The more research and online communities I dove into, the more I found that many women had to fight to get their diagnosis, let alone treatment. I learned that I had to be my own advocate.
Based on my experience, what I can recommend is this:
- Look into the symptoms of PCOS and see if any are applicable to you. If so, talk to your doctor about getting testing. It never hurts to be sure.
- In addition to that, if you’re thinking about getting pregnant, get with your doctor and see if there are any testing or lifestyle changes that need to be done prior. It would have been so much more helpful to know this sooner rather than later.
- And of course, advocate for yourself. I wasn’t happy with my doctors, and I should have changed my PCP. I should have asked for a referral to an RE, maybe even seen another gyno. I should have stood up for myself.
Three years later I’m doing a lot better. The weight loss portion is still a challenge, but I have a much better healthcare team behind me and I’m more informed.
Additional Resources
- How Women’s ‘Health-Care Gaslighting’ Went Mainstream
- PCOS Diva
- PCOS Wellness
- PCOS Diet Support
- The Hormone Diva
- The PCOS Plate
- Dr. Mariza Snyder
You Might Also Want to Read...

Note: This article may contain affiliate links. I only link to products that I know, love, and use. For more info, please view my disclaimers.
JOIN the LIST
Subscribe and stay up to date with the latest blog posts.
JOIN the LIST
Shop My Posts
Want to know where I get #AllTheThings from my blog or Instagram posts? Find what you're looking for below (or just ask).
LIKETOKNOW.IT
Amazon store
Thank you Cristina, this was excellent information. I am sharing it with my girls who were diagnosed with this a couple of years ago after I started reading your blog.
Thanks, Aunt Gigi! I’m glad I can be a helpful resource.
Super informative, well-thought out blog post. Thank you for sharing your journey, sister. <3
Aww thank YOU!
I was diagnosed with PCOS after a year of a non-stop period. I went to three different doctors until I opted to see a reproductive endocrinologist and they diagnosed me with PCOS. I was blessed because I don’t have problems with blood sugar, gluten or cyst (I’ve only had one so far) but weight gain and anovulation have made getting pregnant tough.
I’m glad that you have a great healthcare team behind you now! That is really one of the most important things to have with PCOS.
Wow, that’s crazy having a non-stop period for so long! It sucks you had to go through some many doctors to get a diagnosis. Good to hear you finally got some answers though. And yes, having a great healthcare team is so important!